Plantar Fasciitis or Plantar Heel Pain?
What is Plantar Fasciitis or Plantar Heel Pain
What Exactly is Plantar Heel Pain?
Plantar heel pain (PHP) refers to discomfort typically felt at the bottom of the heel. The traditional understanding has been that this pain is due to inflammation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes. However, current research indicates that PHP is more of a degenerative condition (tendinopathy) rather than an inflammatory one. The plantar fascia plays a crucial role in weight-bearing and walking, helping to absorb the forces exerted on the foot.
Plantar fasciitis implies inflammation this is incorrect and current research suggests otherwise and should be named tendinopathy.
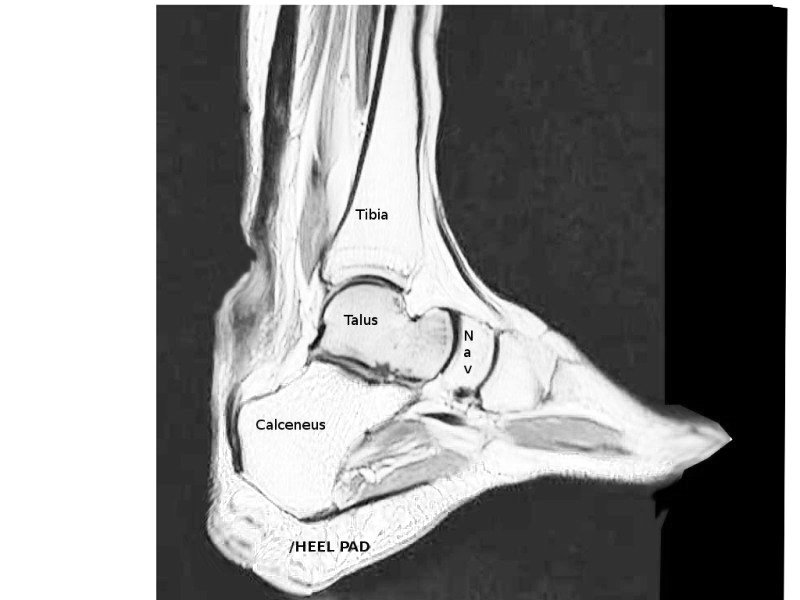
The Anatomy Behind Plantar Heel Pain
At the foundation of foot mechanics is the plantar aponeurosis—a strong, fibrous connective tissue located on the sole of the foot. It comprises three distinct bands: medial, lateral, and central, which work together to support the arches and propel the body forward. When the foot is functioning optimally, the plantar aponeurosis helps distribute the forces of each step, absorbing impact and enabling the foot to spring forward.
One key mechanism involved is the “windlass mechanism.” As the toes dorsiflex (bend upwards), tension builds in the plantar aponeurosis, similar to winding a winch. This tension aids in forming the arch, providing stability during walking. When this balance is disrupted, whether due to improper foot mechanics, repetitive impact, or excess stress, the plantar fascia may develop micro-tears, leading to degeneration and heel pain.
Plantar heel pain (PHP), commonly known as plantar fasciitis, is a condition that has perplexed medical professionals and patients alike for centuries. The terminology surrounding this condition has evolved, with historical references as bizarre as “Gonorrhoeal Heel” in the 1600s. Today, terms like “runner’s heel,” “heel spur,” and “plantar fasciopathy” are used, though “plantar fasciitis” remains the most recognized. However, many experts now argue that the term “Plantar Heel Pain” is more accurate, given that not all cases involve inflammation of the plantar fascia. Let’s explore the complexity behind this condition, including diagnosis, treatment options, and the latest research.
Plantar Fasciitis Symptoms
Symptoms of plantar fasciitis may vary, depending on the severity and duration of the condition. It is important to recognise the various manifestations of foot pain in order to better understand its underlying causes and seek appropriate treatment.
Here are some common symptoms associated with plantar fasciitis:
Heel and Arch Discomfort: The most evident signs of foot pain often include sensations of dull or sharp discomfort in the heel and/or arch of the foot. The intensity of the pain might vary, with some individuals experiencing a constant ache while others endure intermittent bouts of sharper pain.
Burning or Stabbing Sensations: Many individuals with foot pain may experience a burning or stabbing sensation in the affected area, further exacerbating their discomfort. This sensation may come and go intermittently or persist for prolonged periods.
Aggravation with Activity: Foot pain can particularly escalate after prolonged standing or walking. Engaging in activities that put excessive strain on the feet can intensify the pain, making it challenging to continue these activities without discomfort.
Stiffness and Tenderness: Those suffering from foot pain often experience stiffness and tenderness, making it difficult to move or flex the foot as freely as before. Simple actions like bending or flexing the foot might trigger discomfort, reducing mobility and hindering daily activities.
Presence of Lump or Knot: In some cases, individuals may notice the formation of a lump or knot in the arch of the foot. This can be an additional source of distress and may contribute to feelings of discomfort and restricted movement.
Clicking or Popping Sensations: Foot pain can also manifest as clicking or popping sensations within the foot. This unusual sensation may occur during movement and can be linked to various underlying causes.
Sole Pain and Difficulty Weight-Bearing: Individuals afflicted with foot pain often report notable discomfort beneath the soles of their feet, aggravating their ability to bear weight. This can further impede their daily activities, causing frustration and decreased mobility.
Plantar Fasciitis Causes
Plantar Fasciitis is a common condition characterised by inflammation or irritation of the plantar fascia, a thick band of tissue running along the underside of the foot. While the exact cause of this inflammation remains unclear, several factors have been identified as potential contributors to its development:
Repeated strain on the Plantar Fascia: Participating in activities such as running, jumping, or standing for extended periods of time can subject the plantar fascia to repeated stress. Over time, this strain can lead to irritation and inflammation of the tissue.
Age-related degeneration: As we age, the plantar fascia may weaken and become more prone to injury due to reduce activity and motion at the joints in the feet. The natural degenerative changes that occur in the body can make the tissue susceptible to inflammation when subjected to strain.
Foot structure abnormalities: Certain foot structures, such as flat feet or high arches, can increase the stress placed on the plantar fascia. These abnormalities alter the distribution of weight across the foot, creating imbalances that put additional strain on the tissue.
Obesity or sudden weight gain: Excessive body weight can place added pressure on the feet, leading to increased stress on the plantar fascia. This can exacerbate existing foot problems and contribute to the development of plantar fasciitis.
It is important to emphasise that plantar fasciitis can potentially occur in individuals of all ages, activity levels, or body weights. It is not exclusive to athletes or individuals with a specific demographic profile. It is advisable for anyone experiencing symptoms of plantar fasciitis to seek professional medical advice from a healthcare practitioner, either through in-person consultation or online platforms, to determine the underlying cause and establish an appropriate treatment plan.
Risk Factors for Plantar Fasciitis
While plantar fasciitis can affect anyone, there are certain factors that can contribute to an increased risk of developing this condition. These factors include:
Physical Activity: Engaging in high-impact activities such as running, jumping, or dancing can put a significant strain on the plantar fascia, increasing the chances of developing plantar fasciitis.
Prolonged Standing or Walking: Spending long periods standing or walking, particularly on hard surfaces, can contribute to the development of plantar fasciitis. The continuous pressure on the plantar fascia can lead to inflammation and discomfort.
Foot Structure: Individuals with flat feet or high arches are at a higher risk of developing plantar fasciitis. The biomechanical abnormalities associated with these foot types can increase the strain on the plantar fascia and lead to the development of the condition.
Age: The risk of developing plantar fasciitis tends to increase with age. As we get older, the elasticity and strength of the plantar fascia diminish, making it more susceptible to injury.
Obesity or Sudden Weight Gain: Excess body weight puts added pressure on the feet, which can strain the plantar fascia and lead to inflammation and pain. People who are obese or experience sudden weight gain are more prone to developing plantar fasciitis.
If you have one or more of these risk factors, it is crucial to take proactive steps to prevent the development of plantar fasciitis. This may involve wearing appropriate footwear that provides adequate support and cushioning, taking breaks during physically demanding activities to give your feet a rest, and maintaining a healthy weight to reduce the strain on your feet.
If you are experiencing symptoms of plantar fasciitis, it is recommended to consult with a healthcare professional. They can help determine the underlying cause of your symptoms and develop an appropriate treatment plan tailored to your specific needs. At The Body Lab, we can assist with diagnosis and treatment through our in person or virtual consultations. We are dedicated to providing comprehensive care to individuals suffering from plantar fasciitis and helping them find relief from their symptoms.
Diagnosis of Plantar Fasciitis
Symptom Assessment:
If you suspect that you may be experiencing symptoms of plantar fasciitis, it is important to provide a detailed description of your symptoms to your healthcare provider. You will be asked about the timing of the symptoms and any factors that alleviate or worsen the pain.
Physical Examination:
During the physical examination, either in person or through a virtual setting, your healthcare provider will examine your feet. They will carefully assess the condition of your feet and may ask you to stand and walk to evaluate your gait and foot structure. This examination will help in determining the extent of your condition.
Imaging Tests:
In some cases, your healthcare provider may deem it necessary to order imaging tests such as X-rays or an MRI. These tests can help rule out other potential conditions and provide a more detailed visualization of the affected area. By obtaining a clear view, your healthcare provider can make a more accurate diagnosis.
Confirming the Diagnosis:
Once a diagnosis of plantar fasciitis has been confirmed, your healthcare provider can recommend an appropriate course of treatment. Early intervention is crucial in preventing the condition from worsening and promoting a faster recovery. By receiving the correct diagnosis, you can start implementing targeted treatment strategies for effective management of your plantar fasciitis.
Treatment of Plantar Fasciitis
The Importance of an Individualised Treatment Plan for Plantar Fasciitis
When it comes to treating plantar fasciitis, a comprehensive approach involving both self-care measures and medical interventions is typically recommended. It is essential to work closely with a healthcare professional in order to develop a personalised treatment plan that addresses your specific needs and concerns.
In general, the treatment options for plantar fasciitis encompass a range of strategies aimed at relieving pain, reducing inflammation, improving flexibility, and strengthening the foot. Some of the most commonly utilised methods include:
Rest and Activity Modification: One of the initial steps in treating plantar fasciitis is to rest the affected foot and avoid activities that aggravate the condition. By reducing excessive stress on the plantar fascia, this approach can help facilitate healing.
Ice Therapy: Applying ice to the affected area can be beneficial in reducing pain and inflammation. Sometimes ice therapy sessions can aid in providing temporary relief from discomfort but I don’t recommend this a long term practice.
Stretching Exercises: Engaging in specific stretching exercises targeted at the plantar fascia and calf muscles may be as temporary fix but again does not address the underlying issue and alleviate tension in the foot.
Proper Footwear: Wearing appropriate footwear is essential for the management of plantar fasciitis. Your podiatrist will advise shoes that provide adequate arch support and cushioning can help alleviate strain on the plantar fascia. I do not recommend this or inserts as this is a temporary fix and not a long term concept.
Orthotic Devices: Shoe inserts and night splints may offer valuable support by redistributing pressure and reducing stress on the plantar fascia but do not address the underlying issue. Orthotic therapy may helps alleviate discomfort and promotes healing the ligaments or muscles in your feet have stretched excessively and thus unable to maintain your foot structure.
Therapy and Rehabilitation: Engaging in some therapy or other forms of rehabilitation can be highly beneficial for improving flexibility, strength, and range of motion in the foot. Working to restore foot function can help.
Take charge of your health and let us guide you towards a more comfortable and active lifestyle. Together, we can develop an individualized treatment plan that suits your needs, ensuring you receive the best care possible. You can also review our free exercises to help with plantar fasciitis.
A Shift in Understanding: PHP as a Tendinopathy
Recent research indicates that PHP resembles tendinopathy, a condition characterized by tissue degeneration rather than inflammation. This understanding shifts the focus from using anti-inflammatory treatments like corticosteroid injections to addressing the underlying mechanical issues.
Treatment Options: What Actually Works?
Addressing PHP requires a holistic approach, as simply masking symptoms may not lead to long-term relief. Here are some effective treatment options:
1. Movement Therapy
• What It Is: Movement therapy involves retraining the body to move in ways that reduce stress on the plantar fascia.
• Why It Helps: Correcting improper movement patterns, such as overpronation or heel-striking, can alleviate pressure on the plantar fascia.
• Recommendation: At The Body Lab, movement therapy focuses on whole-body integration, teaching the foot, hips, spine, and core to work in unison.
2. Acupuncture
• What It Is: A traditional Chinese medicine technique that uses thin needles to stimulate specific points on the body.
• Why It Helps: Acupuncture may improve blood flow and reduce tension in areas related to heel pain, promoting natural healing.
• Recommendation: Acupuncture sessions at The Body Lab address not only the foot but also other interconnected areas, such as the lower back and legs.
3. Biomechanical Analysis
• What It Is: A comprehensive assessment of foot and gait mechanics to identify any abnormalities or compensations.
• Why It Helps: Correcting misalignments or dysfunctions helps redistribute forces more effectively across the foot.
• Recommendation: The Body Lab performs detailed gait and movement assessments, creating a customized treatment plan for optimal recovery.
4. Stretching and Strengthening
• What It Is: Targeted exercises for the calf and plantar fascia.
• Why It Helps: These exercises help restore flexibility and strength to the affected area.
• Recommendation: Incorporate heel raises, calf stretches, and toe curls into your routine.
5. Orthoses and Taping
• What They Are: Orthotic insoles and therapeutic tape provide temporary support.
• Why They Help: They redistribute load away from the plantar fascia.
• Limitations: These are short-term solutions and should not be solely relied upon for long-term relief.
6. Resistance Training
• What It Is: Strength training exercises targeting the foot and lower leg.
• Why It Helps: Progressive loading of the plantar fascia can strengthen it more effectively than static stretching.
• Recommendation: Focus on exercises that involve the entire lower limb for a balanced approach.
Injections and Surgery: The Last Resort
• Corticosteroid Injections: May provide short-term pain relief but do not address underlying causes.
• Botulinum Toxin (Botox): Can be used to relax overworked muscles, but long-term effectiveness remains uncertain.
• Platelet-Rich Plasma (PRP): Involves injecting the patient’s own blood platelets into the affected area to promote healing.
• Surgical Interventions: Reserved for severe cases, surgical options may include plantar fascia release or calf muscle lengthening.
Prevention and Long-Term Management
Preventive measures and maintenance are essential to avoid recurrence:
• Maintain a Healthy Weight: Reducing body weight can alleviate stress on the feet.
• Choose the Right Footwear: Opt for shoes that offer adequate support and allow for proper foot movement.
• Stay Active with Caution: Gradually increase physical activity levels and listen to your body’s signals.
• Regular Movement Assessments: Periodically reassessing gait mechanics can help identify and correct potential issues early on.
The Body Lab Approach: Why Choose Us?
Most patients come to The Body Lab after trying other treatments like orthotics or physiotherapy that focus solely on symptoms. Here, we take a different approach:
• Holistic Treatment: We integrate movement therapy, acupuncture, and biomechanics, addressing the whole body’s interconnectedness.
• Tailored Care: Each session is customized based on individual movement patterns and specific needs, ensuring a more comprehensive solution.
• Focus on Long-Term Relief: By targeting the root cause, we aim for sustainable results rather than temporary fixes.
Conclusion:
Understanding Plantar Fasciitis and its Treatment
Plantar Fasciitis is a prevalent foot condition that can cause significant pain and discomfort, primarily affecting the heel and arch of the foot. Although the exact causes of this condition are not always clear, there are numerous treatment options available to manage symptoms and promote healing.
If you are experiencing any symptoms associated with plantar fasciitis, it is crucial to seek medical attention. Consulting with a healthcare professional will help determine the underlying cause and develop an appropriate treatment plan tailored to your needs. Early intervention plays a vital role in preventing the condition from worsening and facilitating a faster recovery.
In addition to seeking medical help, taking preventive measures can significantly reduce the risk of developing plantar fasciitis as well as other foot-related issues. Maintaining a healthy weight, wearing proper footwear that provides adequate support and cushioning, and engaging in stretching exercises before physical activities are effective ways to safeguard against this condition.
It is essential to understand that caring for your feet should be a fundamental part of your overall health and well-being. By dedicating proper care and attention to your feet, you can ensure their health and keep them pain-free for many years to come. Remember, prevention is always better than cure, so prioritise the health of your feet and take proactive steps to avoid problems like plantar fasciitis. Your feet deserve the utmost care and attention, as they support your mobility and daily activities.
References
Pollack, A., & Britt, H. (2015). Plantar fasciitis in Australian general practice. Australian family physician, 44(3), 90-91. Monteagudo, M., de Albornoz, P. M., Gutierrez, B., Tabuenca, J., & Álvarez, I. (2018). Plantar fasciopathy: a current concepts review. EFORT open reviews, 3(8), 485-493.
Buchanan, B. K., & Kushner, D. (2017). Plantar fasciitis.
Grecco, M. V., Brech, G. C., & Greve, J. M. D. A. (2013). One-year treatment follow-up of plantar fasciitis: radial shockwaves vs. conventional physiotherapy. Clinics, 68, 1089-1095
Kim M, Choi YS, You MW, Kim JS, Young KW. Sonoelastography in the Evaluation of Plantar Fasciitis Treatment: 3-Month Follow-Up After Collagen Injection. Ultrasound Q. 2016 Dec;32(4):327-332. [PubMed]
Lee TL, Marx BL. Noninvasive, Multimodality Approach to Treating Plantar Fasciitis: A Case Study. J Acupunct Meridian Stud. 2018 Aug;11(4):162-164. [PubMed]
https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951039/
https://pubmed.ncbi.nlm.nih.gov/30078188/
https://bjsm.bmj.com/content/53/3/182

